
A Closer Look at Osteoporosis from an Endocrinologists Perspective
While May is National Osteoporosis Month, it’s important that the conversation about this condition doesn’t stop there!1 Forming healthy habits when you’re younger can actually help prevent or lessen the severity of osteoporosis as you age.2 Crystal Run Healthcare endocrinologist Ila Khanna, MD, answers important questions about osteoporosis to help people learn more about the disease, treatment options, and how to prevent it.
What Is Osteoporosis?
Here are some basic osteoporosis facts:
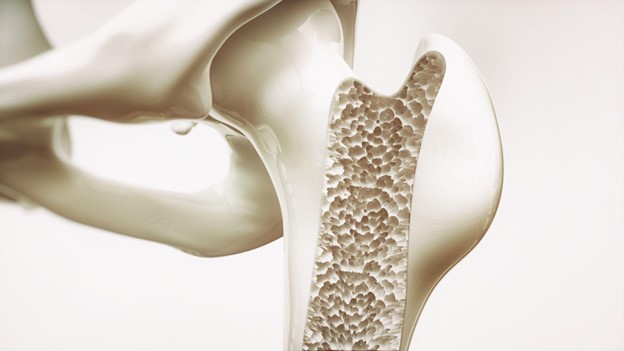 Osteoporosis is a bone disease characterized by inadequate bone mass and advanced deterioration of bone tissue, leading to bone fragility and an increased risk of fractures.3
Osteoporosis is a bone disease characterized by inadequate bone mass and advanced deterioration of bone tissue, leading to bone fragility and an increased risk of fractures.3Osteoporosis mainly affects older women, especially postmenopausal women, and older men. However, it can occur at any age and affect both men and women. There is even a rare form of the disease that affects children (known as juvenile osteoporosis).3,4
Osteoporosis can affect individuals of all races, but it is most prevalent in white (non-Hispanic) and Asian women. Among men, it is most common among those who are non-Hispanic white.3
Osteoporosis is a major health issue, particularly among older adults, contributing to a high incidence of fractures, especially in the hip, spine, and wrist.3
Osteoporosis is the most common bone disease in the U.S. Osteoporosis of the femur neck or lumbar spine affects 12.6% of the population over 50.5
What Are the Symptoms of Osteoporosis?
Osteoporosis is often called a "silent disease," which refers to the fact that symptoms are often unnoticeable until the patient experiences a fracture.3 Because people cannot feel their bones gradually becoming weaker with age, many individuals with osteoporosis do not realize they have this condition.6 Common osteoporosis symptoms include:3
Sudden back pain caused by a fractured vertebra
- Loss of height over time
- A stooped posture
Bone fractures that occur more easily than expected
Fractures can occur from minor falls or from simple everyday activities such as lifting objects or bending over.3
What Are the Causes of Osteoporosis?
 Some important risk factors for developing osteoporosis include:3
Some important risk factors for developing osteoporosis include:3
Age - The risk of osteoporosis increases as you age, particularly after midlife.
Gender - Women, especially postmenopausal women, are more susceptible due to the rapid decline in estrogen levels.
Family History - Persons who have close relatives with a history of osteoporosis are themselves at increased risk.
Body Frame Size - Smaller, thinner individuals are at higher risk because they have less bone mass to draw from as they age. One study has found that men with high levels of body fat are also at greater risk of developing osteoporosis.7
Hormone Levels - Low levels of sex hormones, such as estrogen in women and testosterone in men, can weaken bones.
Dietary Factors - Inadequate intake of calcium and vitamin D can lead to weaker bones.
Lifestyle Choices - Sedentary lifestyle, excessive alcohol consumption, and smoking can contribute to bone loss.
Medical Conditions - Certain conditions, such as rheumatoid arthritis, increase the risk of osteoporosis.
Medications - Use of glucocorticoids, proton pump inhibitors, or certain other medications can contribute to bone loss.
When Should You Get Tested for Osteoporosis?
You should consider getting tested for osteoporosis if:8,9
- You are a woman over age 65.
You are a postmenopausal woman under age 65 with major risk factors for osteoporosis.
More research is needed to recommend osteoporosis screening schedules for men and younger women. Be sure to inform your doctor about risk factors you may have for osteoporosis, including any previous bone fractures and your family history.8
How Is Osteoporosis Diagnosed?
The most common method of testing for osteoporosis is the central dual-energy X-ray absorptiometry (DXA) scan. A type of bone mineral density (BMD) test, it measures bone density in certain areas such as the hip and spine to enable a precise assessment of bone health. Test results take the form of T-scores and Z-scores.10
T-scores and Z-scores are metrics used to interpret bone mineral density test results. A T-score is primarily used for postmenopausal women and older men (50+) to diagnose osteoporosis. It compares the patient’s bone density to the optimal peak bone density of a healthy young adult. A Z-score is more applicable to premenopausal women and younger men.10
There are also other tests, such as quantitative ultrasound (QUS) of the heel and peripheral DXA, which are less comprehensive. Your medical provider will determine the best course of action.10
How Is It Treated?
Osteoporosis treatment often involves a combination of medication and exercise to improve bone health.
Medication
 There are a number of FDA-approved osteoporosis medications. These include:8
There are a number of FDA-approved osteoporosis medications. These include:8
Bisphosphonates - These drugs help preserve bone density and strength by slowing down bone loss, thereby reducing the chance of fractures.
RANK Ligand (RANKL) Inhibitor - Slows bone loss and is used for patients at high risk for fractures or those not responding to other treatments.
Calcitonin - A hormone-derived medication used for postmenopausal women who cannot take other osteoporosis treatments.
Estrogen Agonist/Antagonists - Also known as selective estrogen receptor modulators (SERMs), these are used to treat and prevent osteoporosis in postmenopausal women by mimicking estrogen's positive effects on bone.
Estrogen and Hormone Therapy - These therapies prevent osteoporosis and fractures in postmenopausal women but are recommended for short-term use due to potential side effects.
Parathyroid Hormone (PTH) Analog & PTH-Related Protein (PTHrP) Analog - These increase bone mass and are prescribed for those with severe osteoporosis or high fracture risk.
Sclerostin Inhibitor - Blocks a protein to increase new bone formation and slow bone loss in severe osteoporosis cases.
Exercise
In addition, your medical provider may advise exercises for osteoporosis, such as:8,11
Weight-Bearing Exercises - Activities such as walking, jogging, and dancing help maintain bone density.
Strength Training - Lifting weights or using resistance bands strengthens muscles and bones.
Be sure to follow the advice of your medical provider, as certain types of exercises may be hazardous for persons with osteoporosis.8
How Can It Be Prevented?
 Osteoporosis prevention involves lifestyle choices and dietary adjustments to maintain bone health and density. Here are key methods to prevent bone loss:11
Osteoporosis prevention involves lifestyle choices and dietary adjustments to maintain bone health and density. Here are key methods to prevent bone loss:11
Get Enough Vitamin D
Vitamin D requirements vary from 400 IU to 10,000 IU per day, depending on blood test results. You can obtain vitamin D from sunlight, foods such as salmon, shrimp, fortified milk, or supplements.
Get Enough Calcium
Aim for 1,000 to 1,200 mg of calcium daily through diet or supplements. Good dietary sources include milk, yogurt, cheese, and calcium-fortified foods like cereals and soy drinks.
Stay Active
Exercises such as walking, running, and climbing stairs can combat bone loss. It’s also a good idea to include muscle-strengthening exercises like lifting weights.
Avoid Smoking
Smoking reduces the amount of calcium your body can absorb, which can weaken bones.
Limit Alcohol Consumption
Excessive alcohol intake can weaken bones and increase the risk of fractures.
Adjust Medications If Needed
If you take medicines that cause bone loss, discuss with your medical provider about using the lowest possible dose for the shortest duration.
It’s important to learn how you can help prevent osteoporosis to reduce the chances of serious medical complications. Speak with your primary care physician (PCP) if you have any of the risk factors above. Your PCP will refer you to an endocrinologist if they feel further testing is needed. Remember, start healthy habits while you’re young to help prevent osteoporosis!
Do you see an endocrinologist for osteoporosis? Certainly—and you can find the best doctor to treat osteoporosis right here at Crystal Run Healthcare. Contact us today to learn more about our osteoporosis treatment programs.
Ila Khanna, MD, is an endocrinologist at Crystal Run Healthcare in Monroe. She earned her medical degree from St. George’s University and completed her residency in Internal Medicine at the University of Connecticut in Farmington, CT, and fellowship training in endocrinology at East Carolina University Brody School of Medicine in Greenville, NC. Dr. Khanna is Board Certified in Internal Medicine, Endocrinology, and Diabetes & Metabolism.
Sources:
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Annual Health Observances, Published 10/2024. Annual Health Observances | NIAMS, Accessed 12/2/2024
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Bone Health and Osteoporosis: What It Means to You, Updated 12/2019. Bone Health and Osteoporosis: What It Means to You | NIAMS, Accessed 12/2/2024
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Osteoporosis, Updated 12/2022. Osteoporosis | NIAMS, Accessed 12/2/2024
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Juvenile Osteoporosis, Updated 5/2023. Juvenile Osteoporosis | NIAMS, Accessed 12/2/2024
- CDC. Osteoporosis or Low Bone Mass in Older Adults: United States, 2017–2018, Updated 3/31/2021. Osteoporosis or Low Bone Mass in Older Adults: United States, 2017–2018 | CDC, Accessed 12/2/2024
- Bone Health & Osteoporosis Foundation (BHOF). 25 Facts About Your Bones and Osteoporosis, Published 3/23/2022. 25 Facts About Your Bones and Osteoporosis | BHOF, Accessed 12/2/2024
- Endocrine Society. Men with high levels of body fat may be at risk for osteoporosis, Published 2/10/2022. Men with high levels of body fat may be at risk for osteoporosis | Endocrine Society, Accessed 12/2/2024
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Osteoporosis: Diagnosis, Treatment, and Steps to Take, Updated 12/2022. Osteoporosis: Diagnosis, Treatment, and Steps to Take | NIAMS, Accessed 11/20/2024
- U.S. Preventive Services Task Force (USPSTF). Osteoporosis to Prevent Fractures: Screening, Updated 6/26/2018. Osteoporosis to Prevent Fractures: Screening | USPSTF, Accessed 12/2/2024
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Bone Mineral Density Tests: What the Numbers Mean, Updated 5/2023. Bone Mineral Density Tests: What the Numbers Mean | NIAMS, Accessed 12/2/2024
- Endocrine Society. Osteoporosis, Published 1/24/2022. Osteoporosis | Endocrine Society, Accessed 12/2/2024

 Optum Radiology at Crystal Run Healthcare
Optum Radiology at Crystal Run Healthcare Same and next-day pediatric appointments
Same and next-day pediatric appointments