
Prostate Cancer Screening: What Men Need to Know
Prostate cancer is common, and screening can save lives. The American Cancer Society (ACS) estimates there will be more than 164,000 new cases of prostate cancer and nearly 29,500 deaths from the disease in 2018.1 
The good news is that prostate cancer has very high relative survival rates, even at more advanced stages of the disease (relative survival rates compare men with prostate cancer to men in the general population).2 Nearly 100 percent of men diagnosed with prostate cancer are still alive 5 years after diagnosis, and 96 percent are still alive at the 15-year mark.2
Some of the most celebrated men in the world, including actor Robert De Niro, golf legend Arnold Palmer, and three-time all-star Ken Griffey Sr. have been diagnosed with prostate cancer and lived to tell their stories.
While the outlook is often good for men with prostate cancer—especially when detected early—prostate cancer is still the second leading cause of cancer death (skin cancer is the first) among American men, and 1 in 9 men will be diagnosed in his lifetime.2
Awareness about the disease is critical—understanding your options and knowing the warning signs of a prostate problem can make all the difference. Your urologist can help you understand your risk, which is based on several factors, including age, family history, and lifestyle.
What Is the Prostate, and How Does Prostate Cancer Form?
The prostate is a walnut-sized gland that sits between a man’s bladder and penis. It produces a substance that is released as part of the seminal fluid expelled during ejaculation.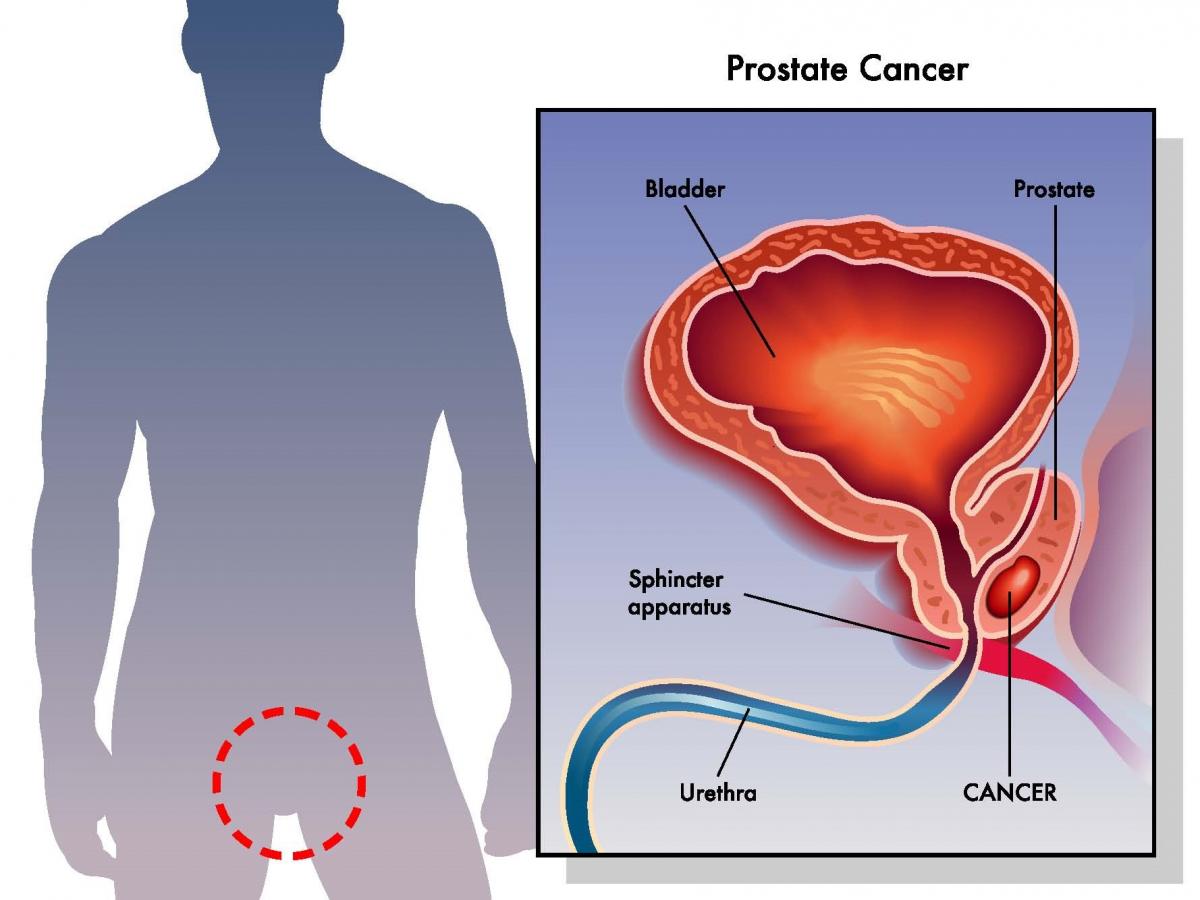
While it’s unclear exactly what causes prostate cancer, we know that, like all cancers, prostate cancer forms because of cellular changes. Normally, the body continually forms new cells and flushes out old or damaged ones; DNA changes (mutations) can lead to the formation of new cells that aren’t needed or prevent old and damaged cells from dying as they should and being flushed from the body. This buildup of cells can lead to the formation of a tumor.
Not all tumors are cancerous. Benign (non-cancerous) tumors are usually localized and non-spreading, and they can usually be removed without coming back. Malignant (cancerous) tumors, on the other hand, can spread to nearby organs and tissues, as well as other parts of the body, and they often grow back.
Prostate Conditions that Are Not Cancer
Certain non-cancerous conditions can mimic some of the symptoms of prostate cancer, which include difficulty urinating, a frequent need to urinate (especially at night), pain or burning during urination, a weak/stop-and-go urine stream, painful ejaculation, and others. These symptoms do not necessarily mean a man has prostate cancer, but they should not be ignored.
Nearly all men experience some degree of prostate enlargement as they age.3 This can impact urination, due to the proximity of the bladder and urethra to the prostate. It’s not uncommon for men to begin having trouble urinating as early as their 30s or 40s. Common non-cancerous prostate problems include:
- Benign prostate hyperplasia (BPH): An enlargement of the prostate that restricts the flow of urine.
- Prostatitis: Infection or inflammation of the prostate gland; there are several types of prostatitis, and symptoms can include chills and fever, repeated bladder infections, pain or discomfort in the groin, or no symptoms at all, depending on the type.
Prostate Cancer Screening Tools
Two of the most common tests used to screen for prostate cancer include:
- PSA Test: When the prostate gland becomes inflamed, enlarged, infected, or affected by cancer, it releases higher-than-normal levels of a protein called prostate-specific antigen, or PSA. Doctors use a simple blood test called a PSA
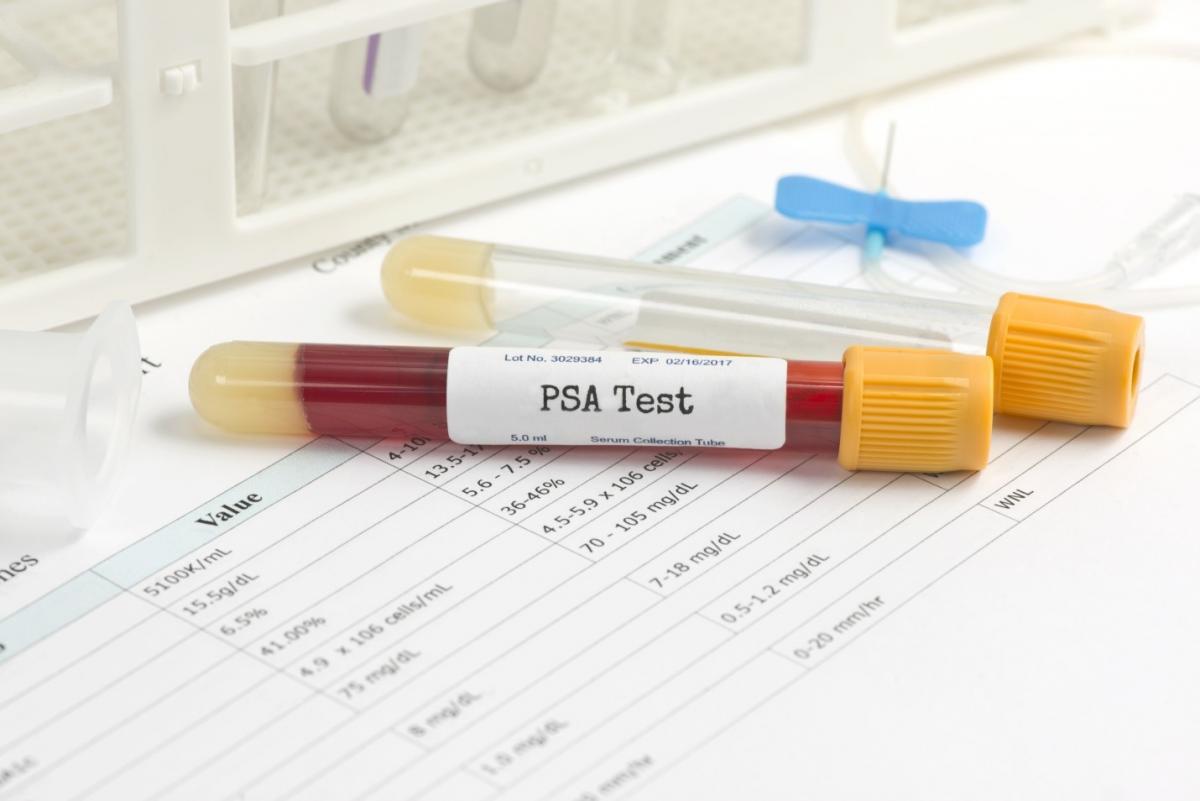 test to check for abnormal PSA levels. It’s important to know that conditions like BPH and prostatitis, as well as other factors like older age, certain medicines, and even ejaculation can raise PSA levels; your urologist can help you understand whether a rise in PSA levels is cause for concern.
test to check for abnormal PSA levels. It’s important to know that conditions like BPH and prostatitis, as well as other factors like older age, certain medicines, and even ejaculation can raise PSA levels; your urologist can help you understand whether a rise in PSA levels is cause for concern. - Digital Rectal Exam (DRE): Some doctors routinely perform a digital rectal exam on patients over a certain age or for those at an increased risk of prostate cancer, such as African American men. The doctor inserts a gloved finger into the rectum to check for lumps, nodules, or other abnormalities and to estimate the size of the prostate.
PSA and DRE test results are reported as a Gleason score, which is used to determine the likelihood that prostate cancer, if present, will spread to nearby tissues.
Additional tests can help detect to what extent, if at all, prostate cancer has spread to nearby bones, organs, and tissues; these include bone scans, computed tomography (CT) scans, and magnetic resonance imaging (MRI) tests.
The Debate over Prostate Cancer Screening
In recent years, the issue of whether, when, and how to screen men who are asymptomatic—meaning having no symptoms—for prostate cancer has been a matter of great interest. The PSA test, in particular, has been the subject of some debate.4,5,6,7
While a PSA test can detect prostate cancer earlier and save lives, it can also produce a false positive or a false negative result; a false positive result indicates disease that doesn’t actually exist, while a false negative result fails to detect disease that is present.
False positives are common with PSA tests—as few as 1 in 4 men with an abnormal PSA test are later found to have prostate cancer. 10
Some prostate cancers grow slowly and never spread beyond the prostate. In these cases, the question becomes whether it’s in a man’s best interest to pursue treatment, assuming a prostate biopsy (usually the next step, if PSA levels are found to be elevated) indicates that cancer is present.
Prostate cancer treatments like radiation, cryotherapy, or prostate removal can result in urinary, bowel, or sexual side effects (e.g., erectile dysfunction) that can seriously impact a man’s quality of life.
Active surveillance/watchful waiting is another option, which involves periodic PSA tests, DRE exams, and (possibly) prostate biopsies. For some men, just knowing that they have an elevated PSA level can be the source of much anxiety. Active surveillance can create additional anxiety—which is why the decision to screen and/or move forward with interventions should be weighed carefully by each patient, under the guidance and support of his doctor.
Different agencies and organizations vary in their recommendations regarding prostate cancer screening. Some organizations have definitive guidelines, while others leave the decision up to men and their doctors.
For example:
- The Centers for Disease Control (CDC) recommends against prostate cancer screening for men who don’t have symptoms.8
- The American Cancer Society (ACA) recommends that men make an informed decision about getting screened based on discussions with their doctor and their own views on the benefits and risks of screening.9
- The American Urological Association (AUA) has specific recommendations, depending on age group and risk factors.10
One thing these organizations have in common is support for informed decision-making.
Informed decision-making happens when a man:
- Fully understands the risks of prostate cancer
- Understands the risks, limitations, and benefits of prostate cancer screening
- Is aware of the alternatives to screening
- Actively participates in the decision-making process about whether to be screened, considering his personal values, feelings, and wishes
When to See a Doctor
It’s never too soon to ask your doctor about prostate health. If you’re experiencing any symptoms of a prostate problem, such as difficulty urinating, a frequent need to urinate at night, burning sensation, or recurring bladder infections, don’t wait—see  your doctor right away.
your doctor right away.
The chances of developing prostate cancer increase significantly after age 50. For this reason, some organizations recommend routine cancer screenings for men age 50 and over, and even earlier for high-risk candidates. Your doctor can help you understand your risk, which is based on factors like age, lifestyle, and family history.
Early detection saves lives. The sooner prostate cancer is caught, the easier it is to treat, and the lower the risk of associated side effects, such as urinary incontinence and erectile dysfunction.
Crystal Run Healthcare: Providing World-Class Urology Care
The esteemed urologists at Crystal Run Healthcare provide comprehensive, compassionate care for men of every age, during every stage of life. Our priority is empowering our patients with the information they need to make informed decisions about their healthcare. Our specialists follow the American Urological Association (AUA) guidelines10 for the early detection of prostate cancer.
Crystal Run offers urology services at our Middletown, Monroe, Newburgh, Port Jervis, Warwick, Rock Hill, and West Nyack, NY locations.
Sources
- https://www.cancer.org/cancer/prostate-cancer/about/key-statistics.html
- https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/survival-rates.html
- https://www.webmd.com/prostate-cancer/enlarged-prostate#1
- http://www.onclive.com/conference-coverage/ipcc-2015/making-sense-of-the-prostate-cancer-screening-debate
- https://www.health.harvard.edu/blog/time-to-rethink-the-psa-to-test-or-not-to-test-debate-2017092912463
- http://www.latimes.com/science/sciencenow/la-sci-sn-prostate-cancer-screening-20170904-story.html
- https://www.mayoclinic.org/diseases-conditions/prostate-cancer/in-depth/prostate-cancer/art-20048087
- https://www.cdc.gov/cancer/prostate/basic_info/get-screened.htm
- https://www.cancer.org/latest-news/prostate-cancer-screening-faq.html
- http://www.auanet.org/guidelines/early-detection-of-prostate-cancer-(2013-reviewed-and-validity-confirmed-2015)
Outside Links
- 1. http://www.everydayhealth.com/prostate-cancer-pictures/famous-men-who-battled-prostate-cancer.aspx
- 2. https://www.webmd.com/prostate-cancer/advanced-prostate-cancer-16/biopsy-gleason-score

 Optum Radiology at Crystal Run Healthcare
Optum Radiology at Crystal Run Healthcare Request medical records online
Request medical records online