When Do Hemorrhoids Need Surgery?
Hemorrhoids are a painful, yet common condition that affects many adults. Though hemorrhoids can often be treated successfully at home, surgery may be necessary when other methods of treatment fail.
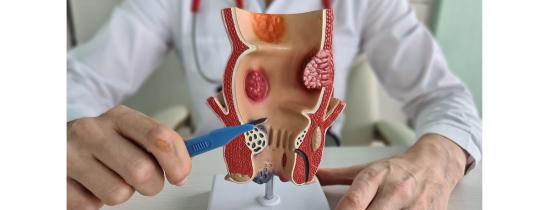
Hemorrhoids Explained
Hemorrhoids are swollen veins located in the anus and lower rectal area. There are two main types of the condition: internal and external.
Internal hemorrhoids can develop deep within anal tissue. Though they may not cause discomfort or pain, internal hemorrhoids can cause internal bleeding. One sign of this condition is observing bright red blood in the toilet following a bowel movement.
External hemorrhoids develop in the anus under sensitive anal tissue. As a result, this type of hemorrhoid often causes pain, itching, and bleeding.
Some people can experience severe pain from hemorrhoids regardless of whether they are internal or external. This is especially true in those who develop blood clots in the affected area, also known as thrombosed hemorrhoids.
Signs That It’s Time to See A Provider About Your Hemorrhoid

While over-the-counter medication or stool softeners may provide some relief, they may not be enough to treat your hemorrhoid pain. If you have tried various at-home treatments, such as eating a high-fiber diet to avoid constipation, with little to no results, it may be time to seek medical help for your condition.
In addition to seeing a doctor for pain relief, there are several symptoms to watch out for that may indicate surgical intervention in needed.
Intense Pain
If you are in so much pain that you’re unable to sit down or evacuate your bowels, it’s time to see a provider for more effective treatments. They may recommend hemorrhoid surgery or an in-office, minimally invasive treatment to relieve your pain and help your hemorrhoids to heal.
Change in Bowel Sensation or Habits
Some types of hemorrhoids can cause you to feel as though you have to evacuate your bowels more often. It may be difficult to clean yourself after a bowel movement, or you may have observed mucous discharge following a bowel movement.
These can all be signs of a prolapsed internal hemorrhoid, which often requires surgical intervention to heal properly.
Prolapsed Hemorrhoid
An internal hemorrhoid can prolapse or migrate outside of the anus when you have a bowel movement. Initially, the hemorrhoid may return to its original position by itself. However, this condition typically gets worse over time. Without intervention, the pain, irritation, bleeding, and itching can intensify significantly. Surgery can eliminate pain and discomfort.
The surgery recommended by your doctor will depend on the type of hemorrhoids you have and their severity. Hemorrhoid severity is classified according to the following grades:
Grade 1 – Hemorrhoid is not prolapsed.
Grade 2 – Prolapse exists, but goes away on its own.
Grade 3 – Prolapse exists, but must be pushed back manually.
Grade 4 – Prolapse exists, cannot be pushed back manually, and is causing significant pain.
What to Expect from Hemorrhoid Procedures
There are several ways to treat hemorrhoids.
Minimally Invasive Treatment Options
Coagulation therapy treats Grade 1 to 3 hemorrhoids by retracting and shrinking them with extreme cold, heat, or infrared light. This procedure is performed in the doctor’s office by inserting a scope into the anal canal to pinpoint and treat hemorrhoids.
Rubber band ligation is a common procedure for those with internal hemorrhoids up to Grade 3. It is done in the doctor’s office. The doctor places a small rubber band around the base of the hemorrhoid to cut off its blood supply. After between two and four procedures, the hemorrhoid shrinks.
Sclerotherapy is another common procedure that is usually completed for those with internal hemorrhoids of smaller size up to Grade 2. This option involves injecting a solution into the hemorrhoid to cause it to shrink and the bleeding to stop. It is performed in a doctor’s office.
Surgical Options to Treat Hemorrhoids

For those with more painful and severe types of hemorrhoids, more invasive surgical procedures may be needed to address them.
Grade 2 and 3 hemorrhoids can be removed via hemorrhoidal artery ligation, which closes off the blood vessels that are causing hemorrhoids using ultrasound.
Hemorrhoidectomy requires hospital admission. This option treats internal hemorrhoid prolapse, large hemorrhoids, and those Grade 3-4 by cutting and removing them. This option is a same-day procedure that requires anesthesia.
Hemorrhoidopexy treats Grade 3-4 hemorrhoid prolapses by installing a surgical staple, which returns the hemorrhoid to its place inside the rectum and cuts off blood supply to the hemorrhoid. This causes the hemorrhoid to shrink and its tissue to be reabsorbed by the body.
This procedure also requires anesthesia, but takes far less time and is less painful during recovery than hemorrhoidectomy.
Manage Hemorrhoids Effectively
Although they can be uncomfortable, painful, and embarrassing, hemorrhoids are very treatable and preventable, both using at-home methods, office-based and surgical procedures. If you have been considering surgical treatment for hemorrhoids, contact the General Surgery department at Crystal Run Healthcare.
Our highly skilled surgeons are fellowship-trained and use state-of-the-art medical equipment to provide a wide range of effective treatments for hemorrhoids of all types and severities. Call 845-703-6999 for more information.

 Optum Radiology at Crystal Run Healthcare
Optum Radiology at Crystal Run Healthcare Same and next-day pediatric appointments
Same and next-day pediatric appointments