What is Age-Related Macular Degeneration? Ophthalmologist and Retina Specialist Dr. Pomykala Explains
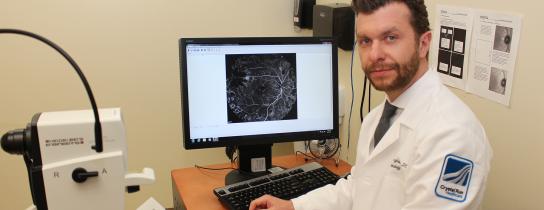
February is Age-Related Macular Degeneration (AMD) month, so we teamed up with Ophthalmologist and Retina Specialist, Matthew Pomykala, DO to find out all about AMD.
What is AMD?
Age-Related Macular Degeneration is deterioration of the retina and deeper layers of the eye that can lead
to a loss in the visual acuity (sharpness) and difficulty with central vision at near and far distances. It is the leading cause of significant visual acuity loss in patients over the age 50 in developed countries.
There are two types of AMD:
- Dry AMD also called non-neovascular is the most common and occurs in 9 out of 10 people with macular degeneration.
Early signs of Dry AMD include small, pale yellow lesions known as drusen forming beneath the retina. The accumulation of these deposits can cause the disease to progress to intermediate and late stages. Subretinal pigment (pigment beneath the retina) changes and large grouped drusen can be classified as Intermediate Dry AMD. A more advanced form of Dry AMD, called Geographic Atrophy, is caused when areas of the central macula (oval-shaped area near the center of the retina) atrophy and thin-out which causesthe loss of cells that are needed for central vision and daily tasks such as reading, watching television or recognizing faces. Significant atrophy is considered an advanced stage of disease and may lead to loss of central vision.
- Wet AMD also called neovasular
Wet AMD is the leakage of fluid or bleeding that can accumulate underneath of within the retina, caused by an abnormal growth of blood vessels beneath the retina. The fluid or blood can occur more quickly and with more serious consequences than the Dry AMD. If not treated the fluid or blood may cause scarring and permanent decline in visual acuity. Patients typically notice blurring, decrease in details, wavy lines or blind spots in central vision. This abnormal growth is known as choroidal neovascularization and it may be a gradual or sudden change.
Most Common Risk Factors:
- Age (over 50)
- Family history of AMD
- Caucasian race
- Cigarette smoking
Other Possible Risk Factors:
- Female gender
- High blood pressure
- High cholesterol
- Light iris color
- Sunlight exposure
- Far-sightedness
- Low dietary fish intake
- Cardiovascular (heart) disease
How do you get diagnosed with AMD?
An Ophthalmologist/Retina Specialist can diagnose you with AMD following a clinical examination in the office with the assistance of diagnostic imaging tools such as Optical Coherence Tomography (OCT), Fluorescein Angiography (FA), Indocyanine Green Angiography (ICGA), and Fundus Autofluorescence (FAF), which help to determine stage of disease and appropriate therapy.
How is AMD treated?
Dry AMD and Wet AMD require different types of treatments. Patients with Dry AMD are encouraged to take nutritional supplements to lower the risk of macular degeneration progressing into more advanced stages. The large research study known as the Age-Related Eye Disease Study 2 (AREDS2) discovered that a specific combination of vitamins and minerals can lower the risk of dry forms and may even lower the risk of progression into wet forms of AMD.
Patients with Wet AMD require treatment with medications known as vascular endothelial growth factor (VEGF) inhibitors that are injected into the eye. These compounds regulate the growth of new abnormal blood vessels in the eye and may stop and reverse neovascularization. There are currently 3 anti-VEGF drugs: Avastin® (bevacizumab®), Lucentis® (ranibizumab®), and Eylea® (aflibercept®). Wet AMD cannot be cured, but its progression may be blocked with the use of these intravitreal, anti-VEGF injections. Prior to the availability of ant-VEGF medications lasers were used with less efficacy to control the disease progression. Anti-VEGF drugs have greatly improved wet-AMD treatment.
References: (www.asrs.org)
Matthew Pomykala, DO, Ophthalmologist and vitreo-retinal specialist at Crystal Run Healthcare, earned his Medical Degree at the University of New England College of Osteopathic Medicine in Biddeford, ME and completed his Residency in Family Medicine & Ophthalmology at St. John’s Episcopal Hospital/Interfaith Medical Center in Far Rockaway, NY. Dr. Pomykala completed Fellowship-training in Vitreo-Retinal Surgery at Associates in Ophthalmology in Pittsburgh, PA and is Board Certified in Ophthalmology. He sees patients in Middletown and Rock Hill.

 Optum Radiology at Crystal Run Healthcare
Optum Radiology at Crystal Run Healthcare Request medical records online
Request medical records online